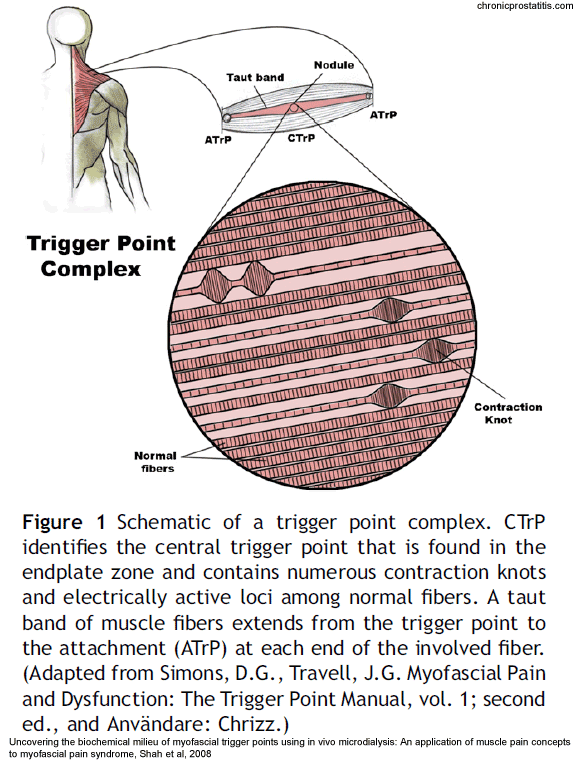
In myofascial pain syndrome, muscle fibers contract but dont release. This creates knots of taut muscle, or trigger points, that send pain throughout the body, even to parts that are perfectly healthy.
Myofascial pain syndrome often leaves doctors baffled and patients untreated
By Amy Mathews Amos
June 17, 2013
My symptoms started in January 2008, with deep pain in my bladder and the sense that I had to urinate constantly. I was given a diagnosis of interstitial cystitis, a chronic bladder condition with no known cure. But in the following months, pain spread to my thighs, knees, hips, buttocks, abdomen and back. By the time my condition was properly diagnosed three years later, I had seen two urogynecologists, three orthopedists, six physical therapists, two manual therapists, a rheumatologist, a neurologist, a chiropractor and a homeopath.
What was wrong? Something completely unexpected, given my symptoms: myofascial pain syndrome, a condition caused by muscle fibers that contract but don’t release. That constant contraction creates knots of taut muscle, or trigger points, that send pain throughout the body, even to parts that are perfectly healthy. Most doctors have never heard of myofascial pain syndrome and few know how to treat it.
In my case, trigger points in my pelvic floor — the bowl of muscle on the bottom of the pelvis — referred pain to my bladder. Points along my thighs pulled on my knee joints, creating sharp pain when I walked. Points in my hips, buttocks and abdomen threw my pelvis and lower spine out of alignment, pushing even more pain up my back. The pain was so severe at times that I could sit for only brief periods.
“Why didn’t anybody know this?” I asked my doctor, Timothy Taylor, soon after he correctly diagnosed the reason for my pain. “Because doctors don’t specialize in muscles,” he said. “It’s the forgotten organ.”
‘There’s no wire’
Most medical schools and physical therapy programs lack instruction in myofascial pain, in part because it involves referred pain, according to Robert Gerwin, an associate professor of neurology at Johns Hopkins University. Gerwin, who is also president of Pain and Rehabilitation Medicine in Bethesda, says that medicine has only recently come to understand this type of pain.
“I remember a long conversation with a neurosurgeon saying that [referred] pain is impossible because there’s no connection, there’s no wire, no string, no blood vessel, there’s no nerve, there’s no nothing connecting these two places,” Gerwin said. Of course, the surgeon was “not realizing that the mechanism of spread is through the spinal cord.”
Pain signals from taut muscle fibers travel to specific locations on the spinal cord that also receive signals from other parts of the body. Referred pain occurs when pain signals from muscles register in the nervous system as if they came from elsewhere.
Although physicians increasingly recognize referred pain today, diagnosis and treatment of myofascial pain often takes more time than most physicians can provide, according to Taylor. Practitioners need specific training to recognize trigger points. And they must examine and palpate patients carefully to identify and locate these taut bands of muscle fiber.
In a 2000 survey, more than 88 percent of pain specialists agreed that myofascial pain syndrome was a legitimate diagnosis, but they differed over the criteria for diagnosing it.
Norman Harden, the medical director of the Center for Pain Studies at the Rehabilitation Institute of Chicago, conducted that survey. He believes that practitioners need clear, validated criteria for diagnosing myofascial pain and identifying effective treatments. He recently conducted another survey to determine if the level of recognition among pain specialists has changed. Preliminary results suggest it has not.
According to Gerwin, myofascial trigger points often cause or contribute to problems such as chronic back pain, headaches and pelvic pain. Trigger points can form anywhere in the body after an injury or if muscles brace against pain or trauma for a long period. They also can result from chronic overuse of muscles due to stress or to poor posture that puts constant pressure on muscles not designed to withstand it.
Taylor understands this as both a physician and a patient. His myofascial pain started in 2003 during his daily run. “I felt a sharp pain in my rear that felt just like when my brothers used to shoot me with our BB gun,” he recalled. He checked himself for signs of injury but found none, then limped home, assuming it was a strained muscle that would heal after a few days. It didn’t.
He sought treatment first from his general practitioner. He then went to a battery of specialists: neurologists, rheumatologists, orthopedic surgeons, osteopathic physicians, physical medicine and rehabilitation specialists, and physical therapists.

